- This is a question asked by all pregnant women - all women worry about whether getting vaccinated might harm their unborn baby.
- The flu (influenza) and whooping cough (pertussis) vaccines have been given to hundreds of thousands of pregnant women and have been shown to be completely safe. Data collected on these women has clearly shown that they are not associated with any increase in birth defects or stillbirths. The benefits to both you and your baby hugely outweighs any theoretical risk from getting vaccinated.
- If you are not up to date with the measles, mumps, rubella (MMR) vaccine, this should be given a month or more before you become pregnant. This is because it is a live vaccine, so cannot be given during pregnancy.
Maternal vaccination in pregnancy
Why are vaccines important for pregnant women?
 Vaccines can help keep you and your growing family healthy.
Vaccines can help keep you and your growing family healthy.- Some vaccine-preventable diseases, such as rubella, can pose a serious risk to your health and that of your developing baby. For this reason, you should make sure that your immunizations are up to date before you become pregnant.
- The antibodies produced when you get vaccinated cross the placenta. This means that when your baby is born, they are already protected against infections, even before they are old enough to get vaccinated themselves. This is one of the only ways of protecting extremely young babies against vaccine preventable infections.
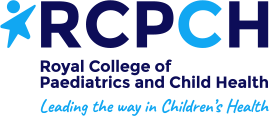
- It is safe, and very important, for pregnant women to receive the inactivated flu vaccine.
- Pregnant women who get flu are at increased risk of severe infection and their babies are also at risk.
- Complications from flu can include premature labour, babies that are small for gestational age, hospitalization, and rarely, death.
- Pregnant women can receive the flu shot at any time during pregnancy. It is normally available from September until around January/February each year.
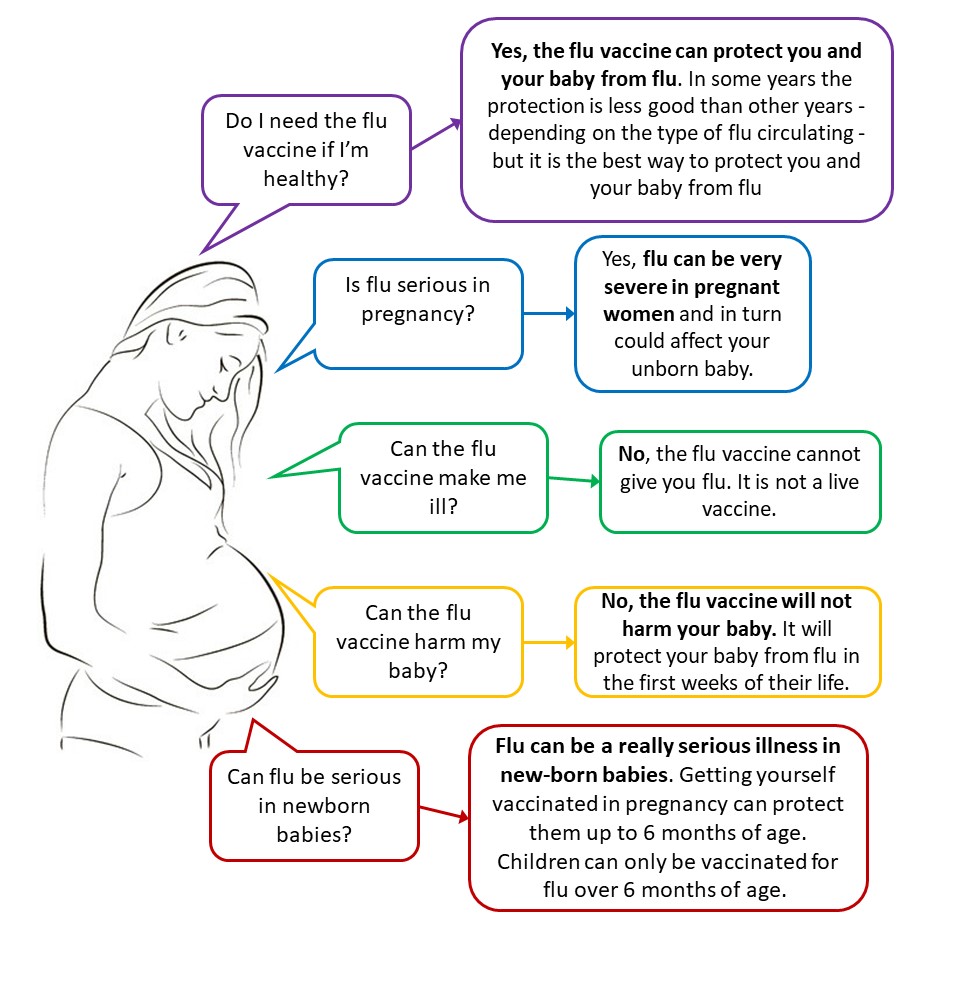
- Whooping cough is one of the most common vaccine-preventable diseases in the United Kingdom. It is caused by bacteria that spread easily from person to person through coughing, sneezing and close contact. It can be very serious for young babies and can cause them to stop breathing and can even cause death.
- The vaccine should ideally be given from 16 weeks, after the foetal scan, up to 32 weeks of your pregnancy.
Click here for more information
From 1 September 2024, pregnant women can have a free vaccine in each pregnancy, to protect their babies against respiratory syncytial virus (RSV).
RSV is a common virus which can cause a lung infection called bronchiolitis. In small babies this condition can make it hard to breathe and to feed. Most cases can be managed at home but around 20,000 infants are admitted to hospital with bronchiolitis each year in England. Infants with severe bronchiolitis may need intensive care and the infection can be fatal. RSV is more likely to be serious in very young babies, those born prematurely, and those with conditions that affect their heart, breathing or immune system.
More information on bronchiolitis can be found here.
How the RSV protects your baby
The vaccine boosts your immune system to produce more antibodies against the virus. These antibodies then pass through the placenta to help protect your baby from the day they are born. RSV vaccination reduces the risk of severe bronchiolitis by 70% in the first 6 months of life. After this age your baby is at much lower risk of severe RSV.
Older children and adults can also get RSV infection, but the disease is more serious for small babies and people aged 75 and over.
The vaccine has been shown to reduce the chance of your baby suffering from severe RSV disease. Like all medicines, no vaccine is completely effective and some babies may still get RSV infection despite their mothers having the vaccine. However, for most babies born to vaccinated mums, any RSV infection should be less severe.
When you will be offered the RSV vaccine
You should be offered it around the time of your 28 week antenatal appointment. If you haven’t heard by this stage, contact your maternity service or GP practice to make an appointment. Having the vaccine in week 28 or within a few weeks of this will help you build a good level of antibodies to pass on to your baby before birth. This will give your baby the best protection, including if they are born early.
You can still have the vaccine later in your pregnancy but it may be less effective. If it wasn’t possible to have your vaccine earlier, it can be given right up until you have the baby. If you have it very late in pregnancy, it may still protect you from infection and reduce the risk of you spreading infection to your newborn baby.
You will be offered the RSV vaccine during every pregnancy
Having the vaccine during each pregnancy will offer your new baby the best protection from RSV.
The safety of RSV vaccination during pregnancy
The vaccine has been studied in clinical trials of almost 4,000 women and been given to many thousands of women in national programmes. Monitoring in the USA, where it has been given to over 100,000 women, has shown a good safety profile. In the main clinical trial, in the month after vaccination, there were slightly more premature babies in the vaccine group (2.1%) than the group that didn’t have the vaccine (1.9%). This difference is most likely to be due to chance.
The vaccine has been approved by medicines regulators in the UK, Europe and USA on the basis of protection, quality and safety.
Babies at a higher risk of RSV infection
Some babies are at higher risk of RSV, such as those who are very premature, those with severe heart disease or those with weakened immunity. They may also be offered an antibody injection. This injection will provide additional protection on top of any antibodies they might get from their mother.
Having the RSV vaccine at the same time as other vaccines
It is important to have your vaccines at the right time in pregnancy
Side effects from the RSV vaccine
The vaccine is a single injection in your upper arm. Side effects are usually mild. These may include:
- headache
- muscle ache
- soreness, redness or swelling at the site of the injection